Intracytoplasmic sperm injection, ICSI, is used to fertilize eggs when there are sperm or egg abnormalities
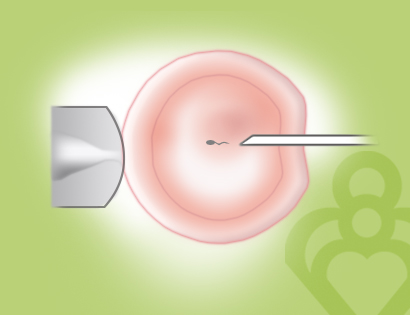 Embryologists use intracytoplasmic sperm injection, ICSI, during in vitro fertilization to fertilize mature eggs when there are sperm or egg abnormalities.
Embryologists use intracytoplasmic sperm injection, ICSI, during in vitro fertilization to fertilize mature eggs when there are sperm or egg abnormalities.
Micromanipulation first saw ICSI in clinical use with IVF for purposes of assisted fertilization in the treatment of male factor infertility, where fertilization potential was low in cases of poor sperm quality. The ultimate evolution of this approach has been the development of the single sperm injection procedure referred to as Intracytoplasmic Sperm Injection, or ICSI.
Using the ICSI technique, the embryologist uses micromanipulation to pick up a single sperm and inject it directly into the egg. This technique is used to fertilize mature eggs in the event of sperm or egg abnormalities.
ICSI is ideal for couples experiencing male factor infertility.
ICSI allows couples with very low sperm counts or poor quality sperm to achieve fertilization and pregnancy rates equal to traditional IVF. It is also recommended for couples who have not achieved fertilization in prior IVF attempts. Sperm of virtually any quality and from any level of the male reproductive tract may be used with the only criterion for use being that the sperm is alive even if it is not moving (motile). Dead sperm may be able to achieve fertilization; however, the DNA or genetic material from such sperm is too degenerate to form a viable embryo.
Immature sperm from the testicle or the epididymis can be retrieved for use with ICSI for men who possess no sperm in their ejaculated semen (azoospermia). This azoospermia is either due to an obstruction in the tract (obstructive), or to extremely low production of sperm in the testicle itself (non-obstructive). In certain cases, men may produce sufficient sperm, but they do not survive to the point of ejaculation (necrozoospermia). Consequently, instead of using non-viable sperm from the ejaculate, testicular biopsy will provide a ready source of freshly produced viable sperm.
ICSI can also be used for non-male factor infertility
The use of ICSI is now routinely applied to a range of clinical situations wherever there is a possibility that conventional in vitro fertilization may be suppressed or not occur. Such situations include the following:
- idiopathic or unexplained fertility
- hyper-responsive ovarian stimulation cases where egg quality may be reduced
- post-thaw sperm samples that survive poorly
- post-thaw egg insemination
- generation of embryos for pre-implantation genetic testing where embryos “clean” from any extraneous contaminating sperm is needed
- any case where there is an extreme need to maximize normal fertilization, for example, when a woman has only a few eggs retrieved
It is possible to “rescue” cases following complete failed conventional fertilization with ICSI. The viability potential of these “late-fertilized” embryos is approximately half of timely fertilized embryos; nevertheless, they do generate successful live births. ICSI has become such a common feature of IVF therapy that it is fast becoming the insemination technique of choice.
Contact our fertility specialists if you would like to learn more about ICSI.


