Minimally invasive gynecological procedures have many benefits
 Has your doctor recommended surgery to give more insight about your fertility issues? This may have initially raised your stress levels to picture yourself in an operating room with a surgeon and a scalpel. However, patients today enjoy less invasive surgical methods that allow them to return back to normal faster. In gynecology, minimally invasive surgery such as laparoscopy and hysteroscopy, have become the norm when women need surgical procedures.
Has your doctor recommended surgery to give more insight about your fertility issues? This may have initially raised your stress levels to picture yourself in an operating room with a surgeon and a scalpel. However, patients today enjoy less invasive surgical methods that allow them to return back to normal faster. In gynecology, minimally invasive surgery such as laparoscopy and hysteroscopy, have become the norm when women need surgical procedures.
In 1988, a pioneering surgeon made medical headlines after making only a 10mm incision in which he inserted a laparoscope (or miniature camera) into a patient’s abdomen and removed a gall bladder. The patient recovered in days, rather than weeks or months. If this patient had undergone traditional surgical procedures of the day in which a large incision was necessary to open up the abdominal cavity, her pain, recovery, and risk of complications would have been much greater.
Since then, minimally invasive procedures have been changing the way people think about surgery, including surgery for gynecological reasons which is generally referred to as minimally invasive gynecologic surgery, or MIGS. Minimally invasive gynecologic procedures use state-of-the-art technology to reduce the damage to human tissue when performing surgery.
Less invasive is better
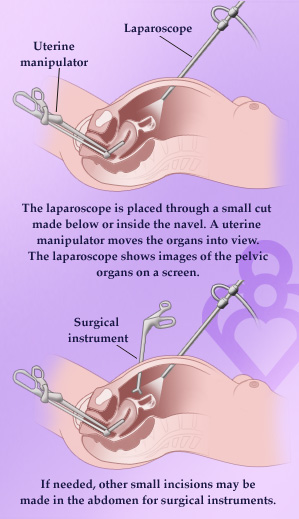
In most procedures, a surgeon makes several small 3/4 inch incisions and inserts thin tubes called trocars. Carbon dioxide gas may be used to inflate the abdominal area, creating a space between the internal organs and the skin. Then a miniature camera is placed through one of the trocars so the surgical team can view the procedure as a magnified image on video monitors in the operating room. Specialized instruments are then placed through the other trocars to perform the procedures.
 Evidence has proven that by using less invasive routes, patients are able to return to normal activities more rapidly. They also experience less pain, bleeding, and infection, and a much shorter hospital stay. For common surgeries such as ovarian cyst removal or evaluation of endometriosis, laparoscopy affords many benefits.
Evidence has proven that by using less invasive routes, patients are able to return to normal activities more rapidly. They also experience less pain, bleeding, and infection, and a much shorter hospital stay. For common surgeries such as ovarian cyst removal or evaluation of endometriosis, laparoscopy affords many benefits.
Benefits of minimally invasive gynecologic surgery
- Quicker recovery – Since a minimally invasive procedure requires smaller incisions than conventional surgery (usually about the diameter of a dime), your body may heal much faster.
- Shorter hospital stays – Minimally invasive procedures help get you out of the hospital and back to your life sooner than conventional surgery.
- Less scarring – Most incisions are so small that it’s hard to even notice them after the incisions have healed.
- Less pain – Because these procedures are less invasive than conventional surgery, there is typically less pain involved.
While minimally invasive surgery may not be right for every woman in every surgical situation, it has been proven an effective alternative to traditional open surgery for the treatments of endometriosis, fibroids, abnormal bleeding, endometrial polyps, mullerian anomalies and ovarian cysts.
Fertility Answers is uniquely qualified to offer our patients with highly-trained physicians in laparoscopic surgery. If your doctor recommends surgery, it’s important to know that you may have options about the way the procedure is done. A great resource for patients who are faced with the need for gynecologic surgery is the MIS for Women website. Also, ask questions and talk to your doctor about minimally invasive surgery so you can get back to life again, quicker and easier.



