An ectopic pregnancy is life-threatening to the mother and cannot lead to live birth
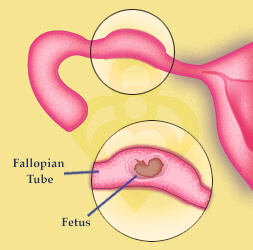
An ectopic pregnancy, or pregnancy that implants in the fallopian tube, is dangerous and life-threatening to the mother. Because the tube is not large enough to accommodate the growing fetus, it will eventually rupture and cause internal bleeding. A tubal pregnancy cannot lead to live birth and if left untreated is life-threatening for the mother.
An ectopic pregnancy happens when a fertilized egg settles and grows anywhere other than the uterus. The vast majority of ectopic pregnancies occur in the fallopian tube (98%) although they can also occur in the abdominal cavity, ovary or the cervix. The major health risk with an ectopic is rupturing of the fallopian tube leading to internal bleeding.
Any disruption of the normal architecture of the fallopian tubes can be a risk factor for ectopic pregnancy. Previous surgery on the fallopian tubes such as tubal ligation or reconstructive procedures, can lead to scarring of the tubes and increases the risk of an ectopic. Likewise, pelvic infections, congenital abnormalities, endometriosis, fibroid tumors or pelvic scar tissue can narrow the fallopian tubes and disrupt egg transportation, thereby increasing the chances.
What are the symptoms of an ectopic pregnancy?
The classic symptoms of an ectopic include acute abdominal pain and vaginal bleeding. However, these symptoms do not mean an ectopic is necessarily present and could represent other conditions. In fact, these symptoms also occur with a threatening miscarriage in non-ectopic pregnancies.
The symptoms of an ectopic pregnancy typically occur six to eight weeks after the last normal menstrual period, but they may occur later if the pregnancy is not located in the fallopian tube. Other symptoms of pregnancy (nausea, breast discomfort, etc.) may also be present in ectopic pregnancy. Weakness, dizziness, and a sense of passing out upon standing can represent serious internal bleeding from a ruptured ectopic pregnancy and require immediate medical attention.
How is an ectopic pregnancy diagnosed?
The first step in the diagnosis is an examination by the doctor. Occasionally, the doctor may feel a tender mass during the pelvic examination. If an ectopic pregnancy is suspected, the combination of blood hormone tests and ultrasound can usually help to establish the diagnosis. Transvaginal ultrasound is the most useful test to visualize an ectopic pregnancy. The ultrasound can also demonstrate the absence of pregnancy within the uterus.
Human chorionic gonadotrophin (beta HCG) blood level tests are also used in the diagnosis of ectopic pregnancy. Beta HCG levels normally rise during pregnancy. An abnormal pattern in the rise of this hormone can be a clue to the presence of an ectopic pregnancy.
How is an ectopic pregnancy treated?
Unfortunately, a tubal pregnancy cannot lead to live birth and must be interrupted and treated. If detected early through either ultrasound or HCG testing, early treatment includes administration of Methotrexate to terminate the pregnancy. After Methotrexate administration, serum HCG levels should be monitored until the HCG level returns to less than 10 mIU/dL.
Ectopic pregnancies left untreated can lead to a rupture of the fallopian tube and internal bleeding, a life-threatening condition for the mother. If you suspect you may have an ectopic pregnancy, please seek medical assistance immediately.


