Patients often have many questions about embryos when they begin an IVF cycle
 Because we can’t see an embryo unless under a microscope, they can be quite a mystery to us. Patients going through in vitro fertilization suddenly start hearing about embryos and may have many questions. How are they created? What stages do they go through before we finally see them as a baby? During in vitro fertilization, how does the IVF lab know if it is a good embryo? What happens to them if we decide to freeze them?
Because we can’t see an embryo unless under a microscope, they can be quite a mystery to us. Patients going through in vitro fertilization suddenly start hearing about embryos and may have many questions. How are they created? What stages do they go through before we finally see them as a baby? During in vitro fertilization, how does the IVF lab know if it is a good embryo? What happens to them if we decide to freeze them?
In this blog post we hope to provide you with all the answers to the questions you have been asking yourself about embryos.
Q: What is an embryo?
A: An embryo is the early stage of development of a multicellular organism. In general, in organisms that reproduce sexually, embryonic development is the part of the life cycle that begins just after fertilization and continues through the formation of body structures, such as tissues and organs. Each embryo starts development as a zygote, a single cell resulting from the fusion of a female egg cell by a male sperm cell.
Q: What happens after fertilization in the early stages of the embryo?
A: In the first stages of embryonic development, a single-celled zygote undergoes many rapid cell divisions, called cleavage, to form a blastula, which looks similar to a ball of cells. Next, the cells in a blastula-stage embryo start rearranging themselves into layers in a process called gastrulation. These layers will each give rise to different parts of the developing multicellular organism, such as the nervous system, connective tissue, and organs. A newly developing human is typically referred to as an embryo until the ninth week after conception, when it is then referred to as a fetus. In other multicellular organisms, the word “embryo” can be used more broadly to any early developmental or life cycle stage prior to birth or hatching.


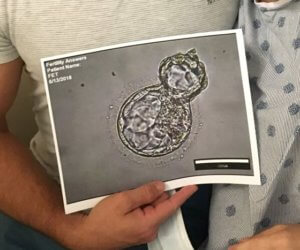
Q: What is the difference between a day three embryo and a blastocyst?
A: An embryo that has been growing for 3 days typically has 8 cells. It is the same size as an egg but the cells get smaller in size as they divide. All the cells are doing the same job and are identical at this point. An embryo that continues to grow to Day 5 becomes a blastocyst with hundreds of cells. The cells start to specialize into different kinds of cells and a cavity forms in the middle which is filled with fluid.
Q: Why are blastocysts important?
A: An embryo that has reached the blastocyst stage at around Day 5 of development has a good chance of making a baby. If an embryo reaches this stage, we know that the embryo is still growing and is a good choice for transfer to the uterus.
Q: What is ICSI?
A: ICSI stands for “Intracytoplasmic Sperm Injection.” Mature eggs are injected with a single sperm on the day of the egg retrieval. ICSI is routinely used to fertilize eggs during an IVF cycle. It is especially useful to overcome many issues surrounding male factor fertility.
Q: When my embryologist talks about normal fertilization the day after my retrieval what does that mean?
A: A normally fertilized egg has 2 pronuclei that the embryologist can view under the microscope. This is referred to as the ‘2PN’ stage. One pronucleus contains the male genetic material and one contains the female genetic material.
Q: What is a morula?
A: A morula is the stage of development before a blastocyst is formed. The cells on day 3 are separate and round and on day 4 they start to squeeze together (compaction) so that the edges of the cells are not clear. This is the morula stage. Fun fact: the name morula is derived from its resemblance to a mulberry and the Latin word for mulberry which is “morum.”
Q: Why do blastocysts have a higher implantation rate?
A: Typically about half of the embryos will continue growing to Day 5. Therefore by watching them grow until Day 5 we are able to get much more information about the viability and quality of each embryo. This helps us to choose the ones more likely to lead to a baby. Biologically, in a natural pregnancy cycle, at around 5 days old the embryo has entered the uterus and is at the appropriate stage for implantation in the uterus.
Q: What is an expanded blastocyst?
A: An expanded blastocyst is an embryo that has grown to 5 or 6 days old and has become a hollow ball of cells taking in fluid from the external environment. The cells have specialized into 2 kinds of cells, baby making cells (inner cell mass) and membrane making cells (trophectoderm).
Q: How does the lab grade embryos, and what is the grading criteria?
A: All clinics have their own grading system, some are similar to others but all grading systems are meant to distinguish between “good, average, and poor” quality embryos. When we talk about “embryo quality” we are only looking at the appearance of the embryo under the microscope. Our laboratory uses the Gardner grading system. Each embryo is assigned a number followed by two letters. The number identifies the stage of blastocyst development, the first letter is the quality of the inner cell mass which becomes the baby, and the second letter is the quality of the trophectoderm which becomes the placenta. Blastocysts are numbered 3-6, with 3 being the least expanded and 6 being the most developed. The inner cell mass and trophectoderm are graded on a scale of ABC with A being the best. The most important information for you to gather about your embryos from the clinician or embryologist is if the embryos are good, average or poor quality.

Q: What is assisted hatching?
A: Assisted hatching is a micromanipulation technique that uses a laser to place a hole in the outer protective shell (trophectoderm) of the embryo before being transferred to the uterus. The use of assisted hatching has been demonstrated to increase implantation rates in cryopreserved embryos. Assisted hatching is also utilized for embryos that will be PGT tested. Assisted hatching allows the embryologist access to the cells that are needed for the genetic analysis.
Q: What is PGT-A?
A: PGT-A stands for preimplantation genetic testing for aneuploidy. This is where a few cells are removed on Day 5 or 6 and the cells are sent to a genetics lab to determine if the embryo has the correct number of chromosomes. It is a known fact that the most common cause of embryo implantation failure is due to an embryo that has the incorrect number of chromosomes. After PGT-A testing, embryos that are genetically normal can be selected for a frozen embryo transfer at a later date. Genetically normal embryos have a high success rate for pregnancy.
Q. What is PGT-M?
PGT-M, or preimplantation genetic testing for monogenetic disease, is another form of embryo genetic testing that can be used to screen an embryo for a known genetic disease such as cystic fibrosis or sickle cell disease.
Q. Can my embryo be damaged during the PGT biopsy process?
Since the cells that are biopsied through PGT come from the trophectoderm (outer shell) part of the embryo, it is highly unlikely to affect the embryo itself.
Q: My embryo PGT report says that my embryo is “aneuploid.” What does this mean exactly?
Humans are designed to have 23 pairs of chromosomes, inheriting one copy of each chromosome from either parent. However, sometimes embryos are formed with too many or too few chromosomes, which is known as aneuploidy. Embryos with aneuploidy may be born with conditions like Down syndrome or Trisomy 21. In many cases, aneuploidy results in either the embryo to not implant or an early miscarriage.
Q: My embryo PGT report says that my embryo is “mosaic.” What does this mean exactly?
As PGT testing has advanced over the past few years, it reveals that not all is black and white with human biology. Indeed, we are finding that some embryos are not one or the other, but can fall on a spectrum between euploid and aneuploid with some having a mix of normal and abnormal cells. This is called mosaicism. Embryos that are mosaic can have different proportions of normal and abnormal cells. A low-level mosaic embryo would have mostly normal cells and a lower percentage of abnormal cells. A high-level mosaic embryo would have mostly abnormal cells and a lower percentage of normal cells.
Q: How are embryos frozen?
A: Embryos are currently frozen using the vitrification technique. Vitrification is a rapid freezing technique that transforms a liquid into a solid glass-like state. This technique does not produce ice crystals within the cell which results in minimal cellular damage during the freezing process. Fun fact: Vitrification is from the Latin word “vitreum,” which means glass.
Q: How are frozen embryos thawed?
A: Frozen embryos are thawed by a rapid warming technique and moved through decreasingly less concentrated solutions to remove the cryoprotectants from the cells before transfer.
Q: What is egg freezing?
A: Mature, unfertilized eggs can be cryopreserved through vitrification on the day of retrieval. The cryopreserved eggs can be stored indefinitely and warmed at a later date to be then fertilized to make an embryo for transfer. Many women choose egg freezing when they want to delay building a family to a later age but want to be able to use younger eggs.
Contact us today to begin your fertility journey.